"*" indicates required fields

22/07/2021
Like other strabismus treatments, the main goal of squint surgery is to correct the misalignment of the eyes. Surgical treatment often improves peripheral vision and cosmetic appearance and may sometimes increase depth perception.
Squint eye surgery is suitable for all ages, from four months onwards. Around 70 to 80% of patients achieve successful outcomes after a single surgery. The remainder may need additional operations to achieve a good outcome.
It’s important to note that strabismus surgery does not correct poor vision or amblyopia, which may require other treatments.
Depending on your individual case, strabismus surgery can be varied and complex. For this reason, it should be performed by an ophthalmologist who specialises in strabismus.
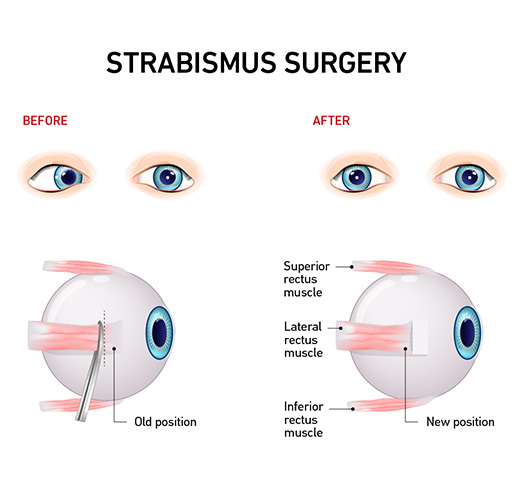
Tightening and loosening the eye muscles during strabismus surgery. (Source: iStock)
Your ophthalmologist will operate only on the eye muscles to straighten the eye. The inner parts of the eye, including those responsible for vision, will not be operated on.
Strabismus surgery is a day procedure that usually takes 30–45 minutes per eye. Typically, children and adults are put under general anaesthesia before squint eye surgery. However, in some cases, adults may be treated under a local anaesthetic.
Once you are asleep, your ophthalmologist will clean around your eye with disinfectant. Your eyelids will be gently held open with a small clamp. Your ophthalmologist will then create an incision in the conjunctiva (the outer surface of the eye) to expose the eye muscle(s) so it can be operated on.
Depending on what is required to align your eye, your ophthalmologist will tighten or loosen one or more eye muscles. Loosening a muscle involves carefully detaching it from the eye and sewing it further back onto the eyeball. Tightening involves cutting away a small piece of the muscle before stitching it back to its original position. The conjunctival incision is then repaired using dissolving sutures.
Where realignment is more difficult, your ophthalmologist may use adjustable sutures to reattach the muscle to the eyeball. These sutures allow the eye to be further aligned several hours after squint eye surgery.
Adjustments are performed while you are awake to improve the cosmetic result and reduce the risk of double vision. Anaesthetic drops are used to make you comfortable while your ophthalmologist makes adjustments.
To help plan for a successful surgery, your ophthalmologist will thoroughly assess your vision, the severity and type of your strabismus and the function of your eye muscles.
They will also ask you about your medical history, to identify any current or past health problems that may affect anaesthesia, surgery, aftercare or recovery. These may include allergies to anaesthesia, antibiotics, other medications and/or surgical tapes or dressings, family reactions to anaesthesia, bleeding or bruising problems, a history of blood clots in the legs or lungs, or poor scar healing after surgery.
Current and past medications and supplements will also be taken into account. Your ophthalmologist may ask you to stop taking some of your medications and supplements before surgery. If this is the case, make sure you thoroughly understand which medications you need to stop taking and when.
You will be required to fast before your surgery.
Most people will be able to go home a few hours after surgery. If adjustable sutures have been used, you will need to wait several hours until the adjustment is complete. A responsible adult will be required to drive you home and someone will need to stay with you for at least a day. Once you are at home, you can resume eating and drinking as soon as you are ready.
In the days following surgery, you may experience some discomfort. Nausea and vomiting may occur after surgery. You may be given anti-nausea medication before surgery to help manage this. Your eyelids may be difficult to open for the first few hours and your eyes could feel sore or irritated for 24 hours or more. They may be bloodshot, watery and/or crusty with a very small amount of blood in your tear fluid on the first day. A headache is not uncommon and should pass within a couple of days.
You will be given medications to help you recover from surgery. These may include pain medications, antibiotic eye drops to reduce the risk of infection, and steroid eye drops to aid recovery. You will be shown how to use your medications before you leave the hospital.
About 30% of older children and adults experience double vision after surgery, which typically passes within about 4 weeks.
Eye surgery is generally very safe. However, in rare cases, complications may occur.
Complications may include (but are not limited to):
It’s important to make an informed decision about whether strabismus surgery is right for you. You should consider the benefits, expected outcome and risks of squint eye surgery versus not having surgery. Your doctor can provide detailed information, answer your questions and help you make a decision.
The anticipated cost of surgery will also be discussed with you. Ask your ophthalmologist for an estimate including surgical, anaesthetic and hospital fees. Note that this will be an estimate only, as sometimes additional, unplanned treatments are needed.
Your ophthalmologist can also tell you how much of the cost is likely to be covered by Medicare and private health funds.
The information on this page is general in nature. All medical and surgical procedures have potential benefits and risks. Consult your ophthalmologist for specific medical advice.
Date last reviewed: 2021-12-20 | Date for next review: 2023-12-20