10/11/2023
Optometrists: This activity may be logged as self-directed learning for 23min of your required CPD hours (dependent upon your personal learning plan).
GPs: This activity may qualify as self-directed learning for 23min of your required CPD hours (educational activities).
Note: The estimated completion time includes time spent reading this article and the linked journal articles, as well as watching the short video.A 61-year-old woman was referred for cataract assessment due to decreased distance acuity. Her optometrist had noted a myopic shift, with best corrected visual acuities being 6/19 (RE) and 6/7.6- (LE). Grade 2+ nuclear sclerosis with some cortical changes were reported bilaterally.
The patient reported a history of decreasing vision over the previous 6 months, which was not remedied by the use of spectacles. Bright lighting was required to allow adequate reading vision, and she also gave a vague account of being told by an optometrist about 15 years earlier that she may have keratoconus in the right eye. She suffered from hay fever and had a history of eye rubbing.
The patient was taking medication for hypertension, hypercholesterolaemia and hypothyroidism.
Visual acuity: unaided 6/19++ & N5 (RE), 6/15= & <N18 (LE), 6/12= & N5 (binocular).
4-year-old multifocal spectacles with a near addition of +1.50 measuring right pl/-1.00×100 and left +1.00/-0.50×85, corrected vision to 6/19 & N5 and 6/7.5 & N12 respectively.
Subjective refraction: -0.75/-1.25×55 (RE) and +1.50/-0.75×125 (LE), correcting to 6/12+ and 6/7.5- respectively.
Binocular vision testing was unremarkable and IOP measured 11 mmHg bilaterally. Corneae were clear.
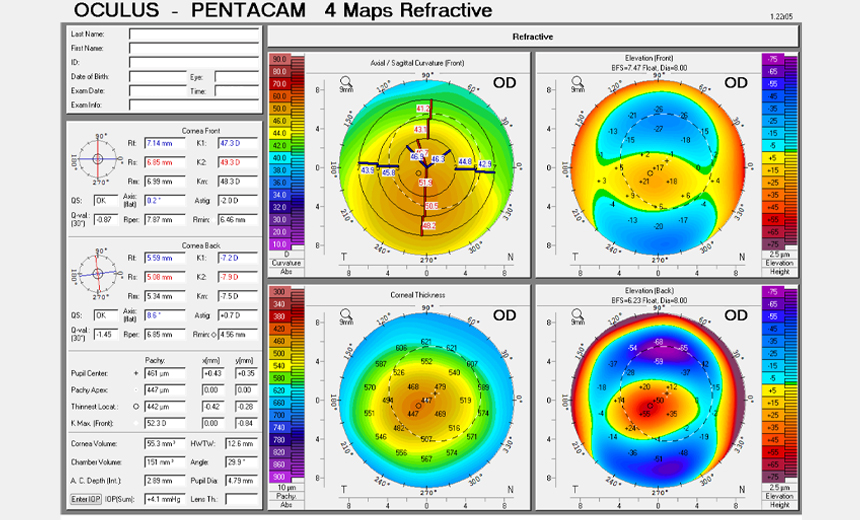
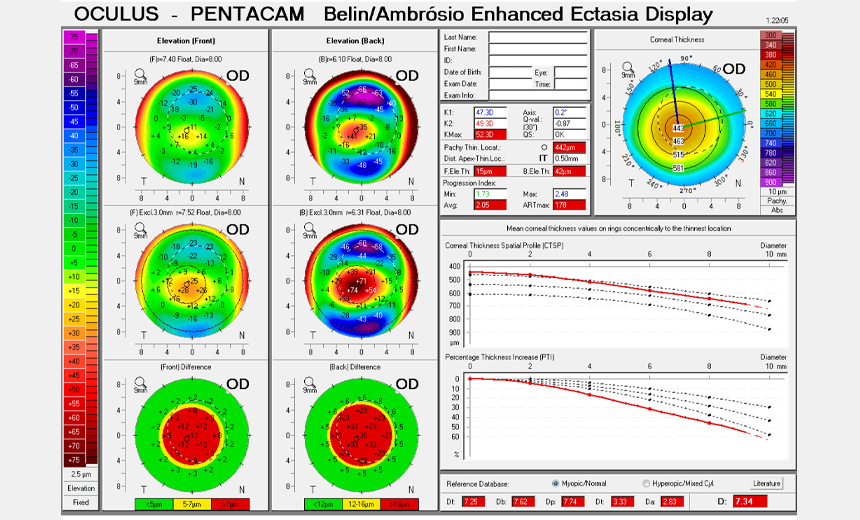
Corneal imaging captured with Pentacam revealed irregular corneal topography in the right eye, with inferior steepening and both anterior and posterior bowing noted on Belin/Ambrosio mapping (Figures 1a and 1b).
The left eye appeared unremarkable (Figures 2a and 2b).
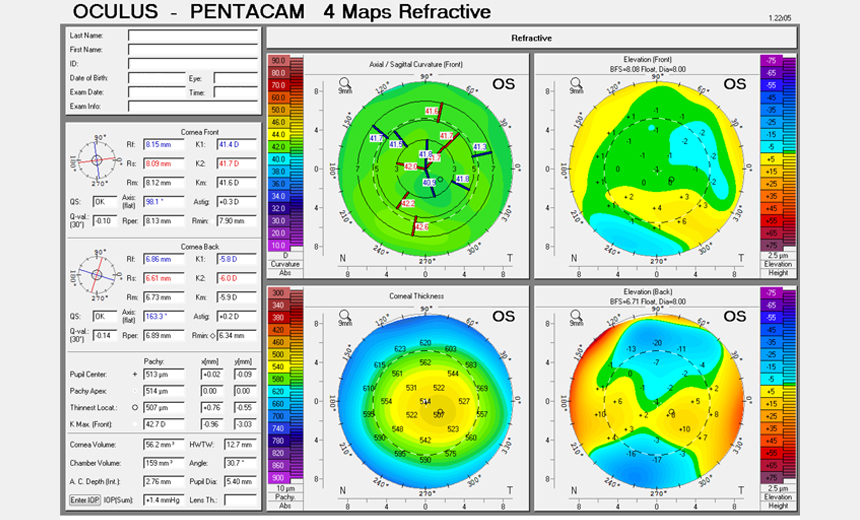
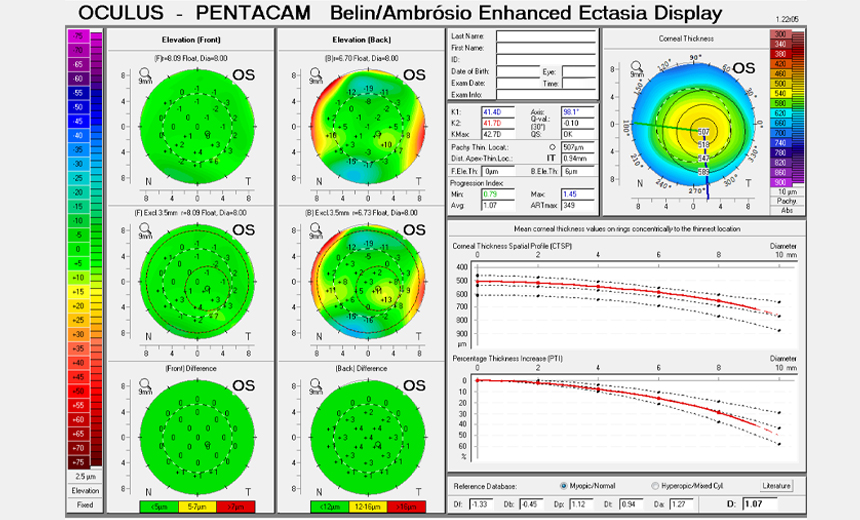
Pentacam Nucleus Staging (PNS) determined that there was grade 1 nuclear sclerosis in the left eye and zero in the right eye. Pentacam scanning also indicated 2 diopters of with-the-rule astigmatism in the right eye and 0.3 diopters in the left. Central corneal thickness was 442 µm in the right eye and 507 µm in the left.
Endothelial cell count was performed, attaining a cell density of 3050.3/mm2 in the right eye and 2982.2/mm2 in the left eye.
An optical coherence tomography (OCT) scan demonstrated healthy maculae, ganglion cell and retinal nerve fibre layer interpretations. A-Scan biometry was also performed.
Bilateral cataracts. Right keratoconus.
It was decided to aim for monovision, whereby the left (dominant) eye would be corrected for distance and the right (ectatic) eye for near vision.
The patient underwent left and then right uncomplicated cataract extraction, and IOL implantation with Alcon AcrySof IQ toric posterior chamber IOLs (right eye SN6AT4 +17.0 and left eye SN6AT2 +23.50).
Post-operative recovery was unremarkable. At 6 months post-surgery, VA was 6/12+++ in the right eye and 6/6- in the left eye. Binocularly, the patient could read 6/4.8 & N5 at near with good lighting.
Approximately 3 years after initial presentation, the patient’s unaided vision was largely stable at 6/12 in the right eye and 6/4.8 in the left eye. Binocularly, the patient could read 6/4.8. Unaided reading vision was N5 in the right eye, N16 in the left eye and N5 binocularly. A small subjective refractive correction was found on the right eye only, measuring pl/-0.75×70. This did not improve the BCVA. IOP was again normal, OCT scanning was unremarkable, and Pentacam imaging of the cornea was stable relative to previous scans.
The patient was reminded not to rub her eyes, and was encouraged to return in 2 years for regular review.
Keratoconus (KC) is typically a progressive condition, where structural weakening of corneal tissue leads to bulging and irregularity, resulting in visual distortion.1 As with most ocular conditions, the ramifications of corneal ectasias lie within a spectrum of severity, with varied patient outcomes. Due to the subjective nature of visual interpretation, along with a broad range of clinical signs, symptoms of KC can easily be attributed to other ocular pathology if not considered carefully.
Originally referred for a cataract assessment, this patient exhibited reduced vision in her right eye in the presence of a shifting prescription, coupled with a nuclear sclerotic cataract. This could have been diagnosed as a simple case of cataract and managed accordingly, if not for a thorough assessment and corneal work-up.
Because this patient was 61 years old with no keratoconic changes of note in the left eye, it was thought that the right-sided KC was already stable at presentation, but the patient was counselled regarding the potential for further deterioration that may warrant collagen cross-linking.2,3 Indeed, there have been documented cases of progressive keratoconus during the seventh and eighth decades of life.4
This finding of right KC, which was incidental during the process of cataract assessment, influenced the IOL selection. IOL selection aimed at left emmetropia and a degree of right monovision, with the understanding that clear reading may not be achieved and that there may be a need for reading glasses.
As well as appreciating that a multifocal IOL would not have been suitable for this patient,5 further consideration was afforded to lens power calculations given the high degree of corneal astigmatism in the right eye. While a T5 IOL was suggested by Barrett calculations (accounting for average K readings across the entire cornea), it was decided that a reduced astigmatic correction was appropriate for the right eye, guided by topographic interpretation of the central cornea that placed more weight on K readings intersecting the visual axis. The patient’s resulting vision was both on target and very pleasing to her, confirming that corneal steepening was contributing to her right eye’s ability to read at near.
Dr Abi Tenen is a well-respected ophthalmic surgeon, whose expertise includes LASIK, PRK/ASLA, TPK, cataract and lens surgery, keratoconus and collagen cross-linking, implantable contact lenses, corneal inlays, pterygium surgery and . Currently her practice focuses on laser refractive surgery and corneal conditions such as keratoconus.
Read moreKyra Stretton is a Clinical Optometrist at Vision Eye Institute with experience in corporate optometry, general ophthalmology and specialist refractive clinics. She has taken multiple international optometry and allied health volunteer trips.
This article is for educational and informational purposes only and may not be directly applicable to your individual patients.
Date last reviewed: 2024-01-12 | Date for next review: 2026-01-12