Diagnosing dry eye
Ophthalmologists use a combination of tests to diagnose dry eye, including:
- Schirmer tear test: Determines if the eye produces enough tears to keep it moist
- Tear-film osmolarity test: Measures the concentration of various components of the tears
- Tear breakup time: Measures how quickly the tear film evaporates
- Corneal fluorescein staining: Shows any abrasions or scratches on the cornea
- Symptom questionnaires: Helps the ophthalmologist determine the severity of your symptoms
Treating dry eye
It’s important to understand that dry eye can’t be cured – ongoing treatment is required. Early diagnosis and treatment may prevent disease progression.
Inflammation of the surface of the eye is commonly associated with dry eye. Untreated cases can result in pain, corneal ulcers, corneal scars and potentially, though rarely, loss of vision.
Treatment may include the following measures to relieve symptoms and prevent complications:3
- Regular artificial tears: At least three to four times a day
- Blink more often: Especially when spending long times in front of a computer or other electronic devices
- Warm compresses: With either a face cloth or heat bag
- Eyelid hygiene: Keep eyelids clean, especially if they get crusty
- Omega-3 fatty acids: Include plenty of these in your diet (found in oily fish, linseeds, chia seeds, tofu and walnuts; supplements are also available)
- Humidify the room: With bowls of water around the room or a good quality humidifier
- Wear wraparound sunglasses: To stop the tear film from drying out too quickly
- Minimise exposure to heaters/airconditioners: To stop the tear film from drying out too quickly
- Topical steroids: Usually reserved for severe or chronic cases, but do carry a small risk of increasing eye pressure – let your ophthalmologist/optometrist know if you have a family history of glaucoma
- Surgery: To close the ducts draining tears from your eyes into your nose
Newer treatments
These include intense pulsed light and thermal pulsation. However, their effectiveness is yet to be determined. The effect of hormone replacement and anti-ageing therapies on meibomian glands is also being researched, in the hope of discovering new treatments.
- Intense pulsed light (IPL): This treatment is usually associated with hair removal, but it has also been used to reduce inflammation along the rim of the eyelids to boost meibomian gland function.
- Thermal pulsation: Special equipment applies heat and light pressure to the meibomian gland to promote the flow of oil.
Reducing the risk of dry eye
To reduce your risk of developing dry eye, you should:
- Get adequate, good quality sleep (7–9 hours most nights)
- Eat a nutritious, balanced diet with plenty of omega-3 fatty acids, including oily fish (such as salmon, sardines, mackerel and anchovies), flaxseeds, walnuts and chia seeds
- Exercise regularly.
Dry eye can also be caused or exacerbated by Digital Eye Strain. This condition results from screen overuse and affects your vision and eye health.
To protect your eyes from Digital Eye Strain, reduce your use of screens where possible, try to blink regularly when using a screen and follow the 20-20-20 rule (take a 20 second break from your screen and look at an object 20 feet, or 6 metres way, around every 20 minutes). You could also modify your workspace to minimise your risk of Digital Eye Strain.
Clinic team
NSW
Dry eye doctors
QLD
SA
VIC
-

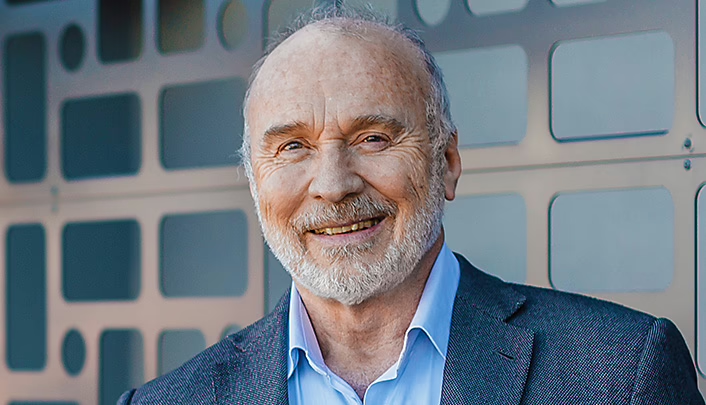
Dr Jeremy Diamond
MB ChB, PhD, FRCS, FRCOphth, FRANZCO
Locations
- Boronia
Book a consultationwith Dr Jeremy Diamond
Dr Philip Hoffman
MBBS(First-class Hons) FRANZCO M Health Ethics Member of ANZSRS
Locations
- Camberwell
- Footscray
Book a consultationwith Dr Philip HoffmanReferences
1. Chia EM, Mitchell P, Rochtchina E, Lee AJ, Maroun R, et al. Prevalence and associations of dry eye syndrome in an older population: the Blue Mountains Eye Study. Clin Exp Ophthalmol. 2003 Jun;31(3):229-32. doi: 10.1046/j.1442-9071.2003.00634.x.
2. Mayo clinic. Dry eyes [Internet]. Scottsdale (Arizona): Mayo Clinic; 2020 [cited 2021 Jan 27]. Available from: https://www.mayoclinic.org/diseases-conditions/dry-eyes/symptoms-causes/syc-20371863
3. American Optometric Association. Dry eye [Internet]. St Louis (Missouri): American Optometric Association;[date unknown] [cited 2021 Jan 27]. Available from: https://www.aoa.org/healthy-eyes/eye-and-vision-conditions/dry-eye?sso=yResourcesThe information on this page is general in nature. All medical and surgical procedures have potential benefits and risks. Consult your ophthalmologist for specific medical advice.
Date last reviewed: 2025-03-17 | Date for next review: 2027-03-17