45-year-old woman with increasing blurred vision and photophobia
18/07/2018
CPD hours
Optometrists: This activity may be logged as self-directed learning for 20min of your required CPD hours (dependent upon your personal learning plan).
GPs: This activity may qualify as self-directed learning for 20min of your required CPD hours (educational activities).
Note: The estimated completion time includes time spent reading this article and studying the figures.History/Presentation
A 45-year-old female was referred for increasing blurred vision and photophobia in her right eye over the preceding week, with reduced foreign-body sensation. She had previously been referred to an ophthalmologist with similar symptoms.
RVA: 6/7.5
LVA: 6/5
- What else is important to ask this patient?
- Recent cold/flu-like illness
- Recent or past history of cold sores
- History of chicken pox and/or shingles (punctate keratitis and small pseudodendrites can occur up to 1/12 after V1 shingles)
- What treatment has previously been given?
- Patient unsure (?steroids, ?Zovirax, ?tablets)
- Request notes from other treating ophthalmologist
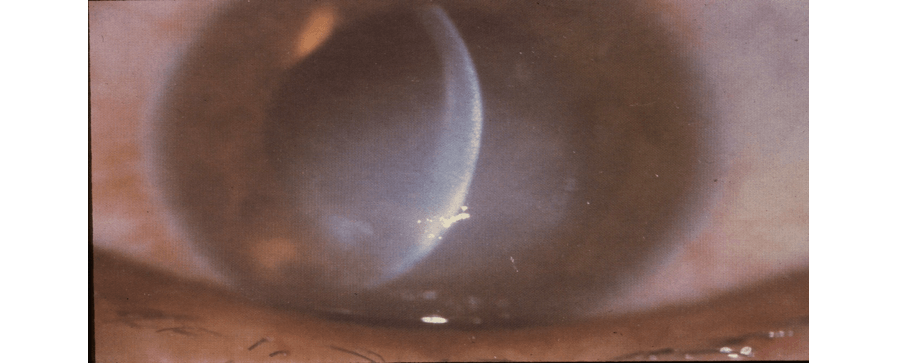
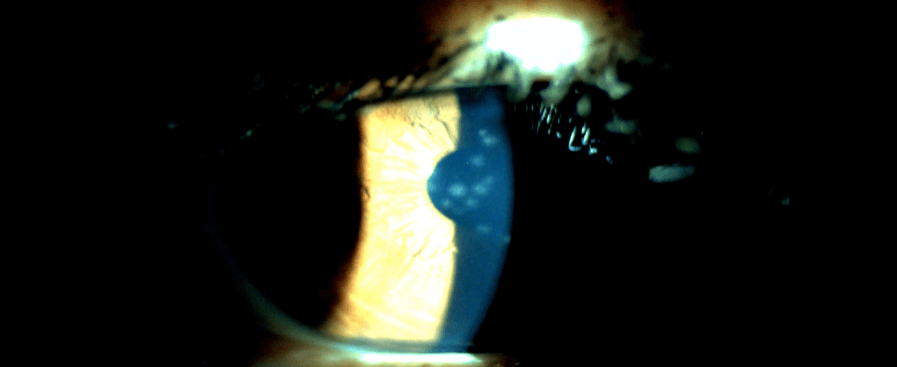
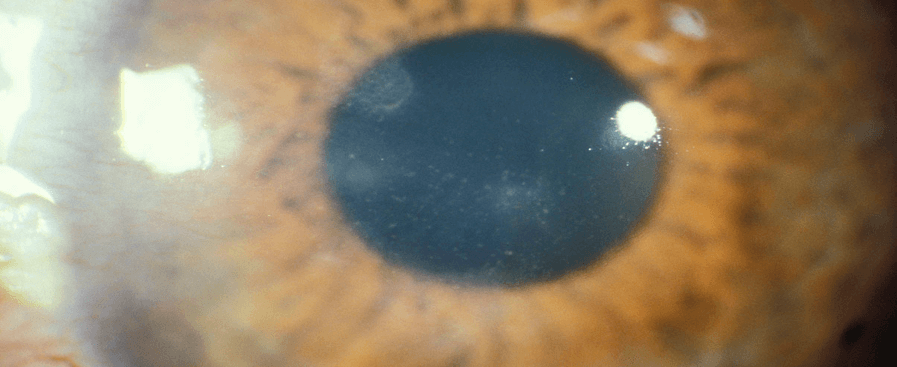
- What can you see?
- Subepithelial haze/nummular keratitis
- 1+ AC cells
- What are the differential diagnoses?
- HSV kerato(uveitis)
- Adenoviral/other viral keratitis (e.g. Epstein-Barr virus)
- Varicella zoster keratitis (history or recent shingles)
- Bacterial/fungal (usually more fluffy with other red flags in patient history)
- What other examination/tests would you like to do?
- Fluorescein staining/eye drops
- Corneal sensation (important in herpetic disease)
- Iris atrophy/transillumination (sectoral versus patchy) – HSV/VZV
- Always check the fundus for retinal/choroidal/vascular abnormalities
The patient reveals a history of cold sores, including a recent flare-up. Approximately 12 months ago, she had seen another ophthalmologist for the same symptoms and the patient notes confirmed she had been treated with Maxidex and Zovirax.
Diagnosis
Given her history and presence of small epithelial defects (but not dendrites), it is highly likely this patient has herpes simplex virus (HSV) keratouveitis.
Treatment
- Start Maxidex (dexamethasone) and taper slowly over 4 weeks (qid, tds, bd, daily)
- Zovirax 3% (aciclovir) ointment cover may decrease the risk of dendritic ulcer developing
- Consider stopping Zovirax after 2 weeks as the risk of epithelial HSV is very low in true herpetic keratitis. Some clinicians only use topical steroids, but it’s probably safer to cover with Zovirax ointment for initial 1-2 weeks.
Oral famciclovir was discussed with the patient as an alternative anti-viral option. Compared to topical Zovirax, oral famciclovir offers quicker resolution of symptoms, less corneal toxicity and some added benefit if uveitis is present. However, the cost is often prohibitive for patients because it is not listed on the PBS for HSV.
Progress
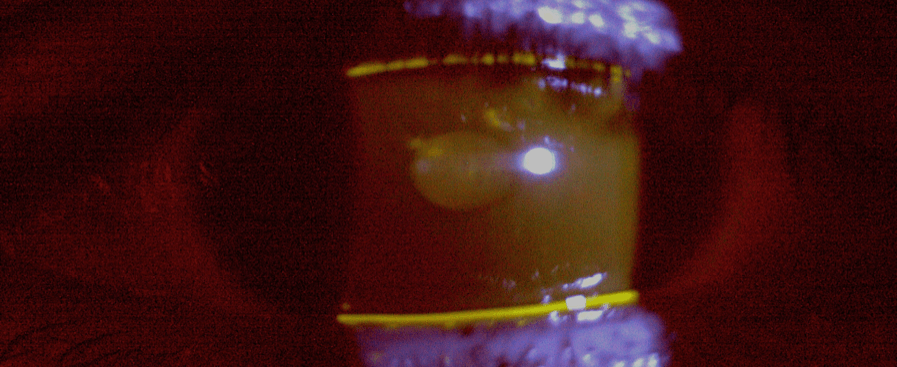
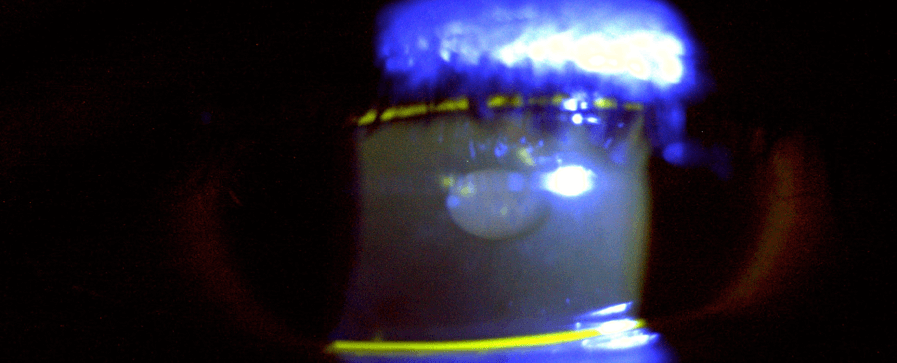
2 weeks after presentation

4 weeks after presentation
Managing HSV recurrence
- Re-commenced topical Zovirax tds
- Initiated Flarex eye drops (fluoromethalone) qid
- Stressed importance of slow taper over 6–8 weeks
- Flarex qid 1/52 with tds Zovirax
- Flarex tds 1/52 with tds Zovirax
- Flarex bd 1/52 with bd Zovirax
- Flarex daily 2 weeks with daily Zovirax
- Flarex alternate days 2 weeks with alternate day Zovirax
The patient was asked to return for a review in 1–2 weeks and again 2 weeks after stopping treatment (or ASAP if symptoms are worsening).
HSV keratitis nomenclature
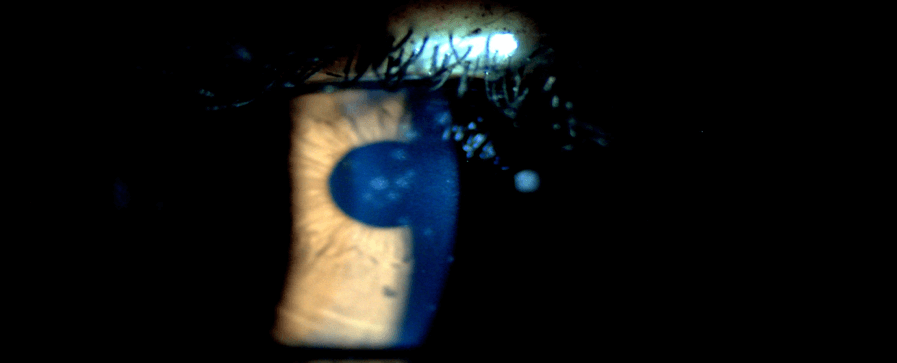
- Epithelium
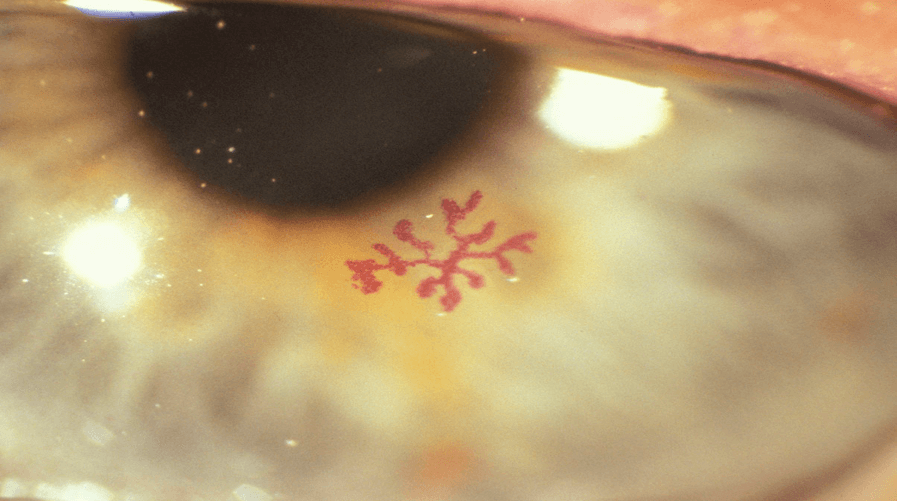
- HSV epithelial keratitis (dendritic epithelial ulcer or geographic epithelial ulcer)
- Stroma
- HSV stromal keratitis without ulceration (non-necrotising keratitis, interstitial keratitis, immune stromal keratitis)
- HSV stromal keratitis with ulceration (necrotising keratitis)
- Endothelium
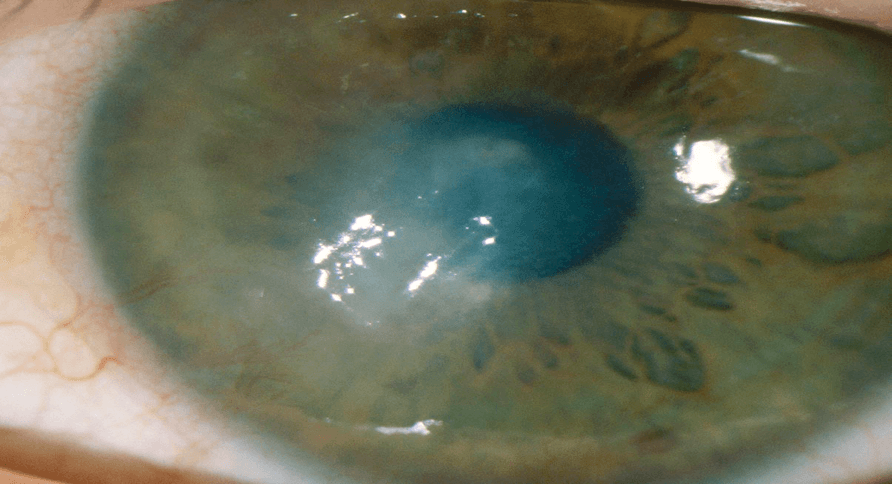
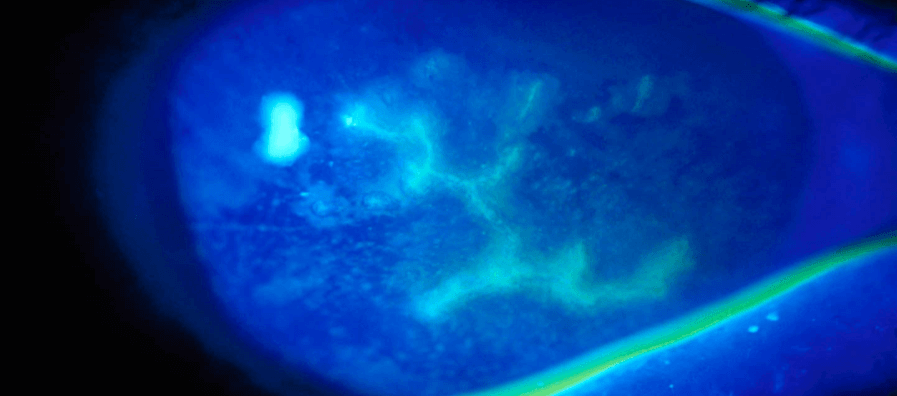
- HSV endothelial keratitis (disciform keratitis)
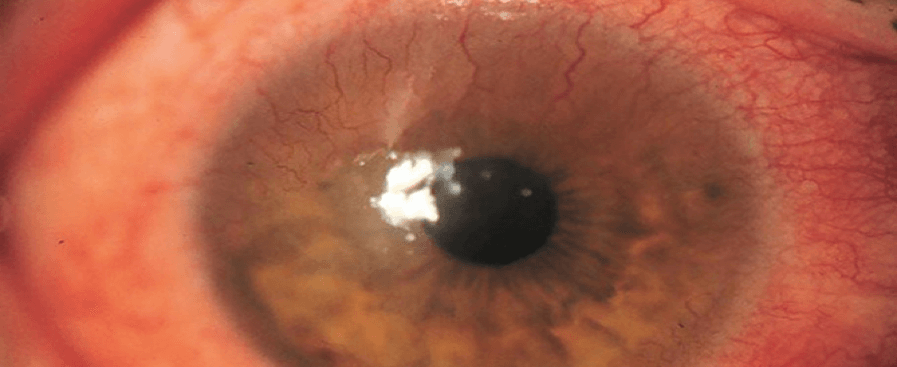
DENDRITIC ULCER
HERPETIC KERATOUVEITIS
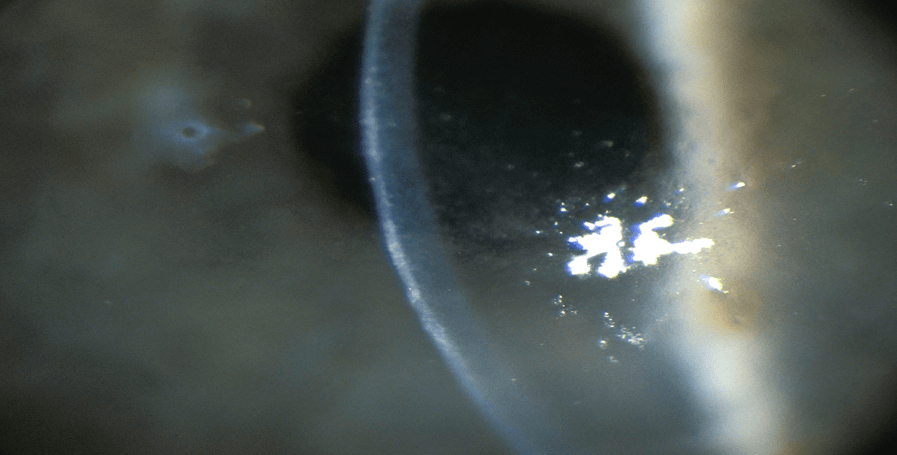
RECURRENT INTERSTITIAL KERATITIS + NEW DISCIFORM
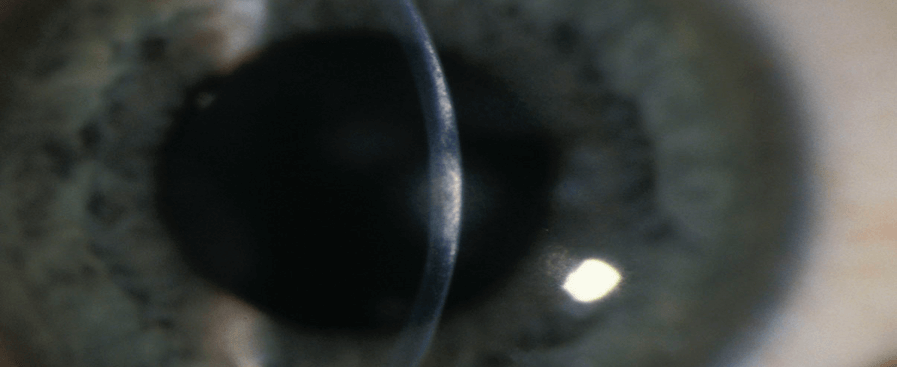
ENDOTHELIAL/DISCIFORM KERATITIS
HERPETIC SCARS
GEOGRAPHIC ATROPHY
HSV keratitis treatment protocol
Epithelial disease only
Topical corticosteroids should be avoided in the initial management of HSV epithelial keratitis.
- Dendritic ulcer
- Debride/debulk: LA-soaked cotton wool rolled over lesion
- Topical acyclovir: 5 times per day day 7/7, tds 7/7 OR
- Oral aciclovir, valaciclovir, famciclovir: 7–10 days then lower dose
- Geographic ulcer
- Topical aciclovir: 5 times per day until healing then tds 7/7
- Watch for toxicity/non healing/worsening, which requires oral Rx
- Intensive gel lubricants (e.g. Genteal Tears)
- Oral antivirals (maximum dose): 2–3/52 (preferred as less corneal toxicity) but are expensive
- Topical aciclovir: 5 times per day until healing then tds 7/7
Stromal disease
- Without epithelial ulceration
- Topical steroids: 4–6 times per day, tapering quickly at first and then more slowly (e.g. by 1 drop weekly for first 3–4 weeks then every second week for next 4–6 weeks)
- May need 6–12 weeks of treatment, depending on response and history
- Oral/topical antiviral cover: lower/prophylactic oral dose of acyclovir or famciclovir or bd–tds topical Zovirax cover
- With epithelial ulceration
- Antiviral cover: topical or oral using therapeutic (higher) dose
- Topical steroids: lower dose (e.g. bd) until ulcer heals then increase as necessary OR
- Withhold steroid for first 24–36 hours of antiviral therapy before commencing lower dose and increasing once ulcer heals
- Taper steroids as above or based on disease response
Endothelial keratitis/disciform keratitis
- Responds more quickly than stromal keratitis
- Initiate therapeutic dose of antivirals for 7–10 days, then drop to prophylactic dose while on steroids
- Topical steroids 4–6 times per day for 7–10 days, then taper over 3–4 weeks based on response
If AC inflammation is severe, steroids may need to be administered more frequently.
HSV long-term oral prophylaxis
Prophylaxis is considered in patients with:
- >1 recurrence within 12 months
- Scar/vascularisation getting close to visual axis
- Pre/post-operative patient with a history of HSV keratitis (e.g. undergoing corneal graft, refractive other ocular surgery)
- Immunocompromised (e.g. on chemotherapy).
Key message:
Herpes viruses, including HSV1, HSV2 and VSV, can all affect the eye. The possible diagnosis of such conditions should always be kept in the back of the mind in any patient presenting with corneal inflammatory changes (oedema, infiltrates, epithelial defect) and/or uveitis. Any patient with suspected corneal herpetic disease must have a dilated exam to look for intraocular involvement.
Dr Nima Pakrou is an experienced ophthalmologist with expertise across a range of eye conditions. His subspecialty areas include medical retinal diseases, cataracts, intraocular inflammation and oculoplastics. He practises at Vision Eye Institute Footscray.
This article is for educational and informational purposes only and may not be directly applicable to your individual patients.
Date last reviewed: 2023-08-14 | Date for next review: 2025-08-14