Multiple evanescent white dot syndrome
22/12/2017
CPD hours
Optometrists: This activity may be logged as self-directed learning for 9min of your required CPD hours (dependent upon your personal learning plan).
GPs: This activity may qualify as self-directed learning for 9min of your required CPD hours (educational activities).
Background
A 42-year-old diabetic patient with a unilateral decrease in visual acuity (VA) and a history of flashes and floaters was referred for suspected retinal detachment. Best-corrected visual acuity (BCVA) was 6/5 in the right eye and 6/36 in the left eye.
Examination
On examination, the patient had a left relative afferent pupillary defect (RAPD) and decreased colour vision. Dilated retinal examination showed no evidence of retinal detachment or diabetic retinopathy, and the optic disc appeared normal. The rest of the physical examination was unremarkable. A provisional diagnosis of atypical optic neuritis was made and further diagnostic tests ordered.
Investigations
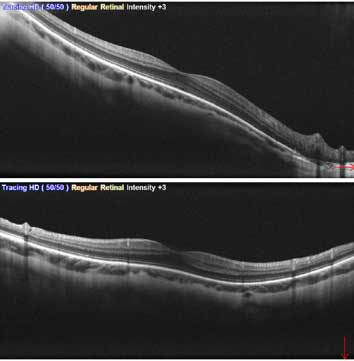
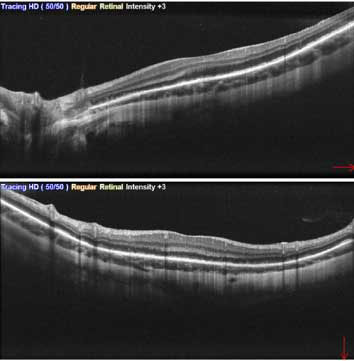
An optical coherence tomography (OCT) scan of the macula showed disruption of the ellipsoid zone.
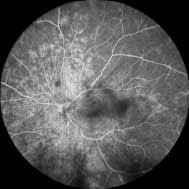
A subsequent fluorescein angiogram (FA) showed early hyperfluorescence in multiple areas and late staining of the optic disc.
12 seconds 
13 seconds 
15 seconds 
25 seconds 
35 seconds 
40 seconds 
2 min 5 sec 
2 min 26 sec 
4 min 22 sec 
4 min 39 sec 
Diagnosis
The patient was diagnosed with multiple evanescent white dot syndrome (MEWDS).
What is MEWDS?
This condition belongs to a group of posterior uveitidies, known as the white dot syndromes. MEWDS is a rare, inflammatory condition of the retina that is seen more commonly in younger females and tends to be unilateral. Patients may recall suffering from a viral illness (e.g. flu-like symptoms) prior to the onset of ocular symptoms, but this is not always the case. As its name suggests, the characteristic finding with MEWDS is the presence of multiple small whitish/yellowish dots throughout the peripheral macula and around the optic nerve. Foveal granularity is another classic sign. Mild vitritis may be present, but the anterior chamber remains unaffected. Optic disc oedema and an RAPD are often observed. OCT demonstrates disruption of the ellipsoid zone, while early hyperfluorescent lesions arranged in a wreath-like pattern are visible with FA.
Symptoms
- Acute, non-painful loss of VA
- Scotomas
- Photopsia
- Dyschromatopsia
Differential diagnoses
- Optic neuritis
- Acute posterior multifocal placoid pigment epitheliopathy
- Birdshot chorioretinopathy
- Acute retinal pigment epithelitis
- Diffuse unilateral subacute neuroretinitis
- Multifocal choroiditis
- Sarcoidosis
- Punctate inner choroiditis
- Serpiginous choroidopathy
- Acute zonal occult outer retinopathy
- Intraocular lymphoma
- Syphilitic chorioretinitis
- Ocular tuberculosis
Treatment
MEWDS is self-limiting so no treatment is required. Baseline visual acuity typically returns within a few weeks or months. Recurrence is unusual. Scotomas, photopsia and dyschromatopsia may persist in rare cases. Lesions may be replaced by scar tissue.
Think of MEWDS in atypical optic neuritis
Dr Raj Pathmaraj is a comprehensive ophthalmologist with significant experience in ocular surface diseases, cataract and refractive surgery, glaucoma and other optic nerve diseases. He consults at Vision Eye Institute Blackburn South.
References
- Raven M, Ringeisen A, Yonekawa Y et al. Multi-modal imaging and anatomic classification of the white dot syndromes. Int J Retina Vitreous 2017;3:12.
- Medscape. White Dot Syndromes (https://emedicine.medscape.com/article/1227778-overview#a4). Accessed online 20 October 2017.
This article is for educational and informational purposes only and may not be directly applicable to your individual patients.
Date last reviewed: 2023-08-14 | Date for next review: 2025-08-14