Diagnosing corneal conditions
If you have pain, redness or swelling in your eye, your ophthalmologist will conduct a comprehensive eye examination. Some tests specifically highlight problems with the cornea. Other tests may help to rule in or rule out non-corneal causes.
- Slit lamp: A microscope with a bright, intense light allows the ophthalmologist to study the cells lining your cornea (endothelial cells) and detect irregular bumps that might indicate Fuchs’ dystrophy.
- Fluorescein eye stain: To accurately diagnose a corneal abrasion or ulcer, your ophthalmologist may perform a fluorescein eye stain. This is a test that uses fluorescent orange dye and a blue light to detect damage to the cornea.
- Conjunctival scraping or biopsy: A sample of cells is taken from the conjunctiva to test for serious bacterial infections, such as trachoma, which is the world’s leading infectious cause of blindness.
- Corneal topography: This is a computer-assisted diagnostic tool that creates a three-dimensional map of the surface curvature of the cornea. It helps diagnose corneal abrasions, deformities and irregular conditions that are not visible with conventional testing.
- Eye pressure test: After numbing your eyes with drops, your doctor will briefly touch your eyes with a special instrument that measures the pressure inside your eye. This test can help distinguish between a disease that increases pressure in your eye (glaucoma) and a corneal condition such as Fuchs’ corneal dystrophy.
- Pachymetry: This is a simple, painless test using a small instrument about the size of a digital thermometer to measure the thickness of your cornea. The test takes less than 30 seconds per eye.
Treating corneal conditions
Corneal abrasion
If you suffer from a scratch or an injury to the surface of your eye, don’t rub your eye or touch your cornea.
If a foreign object is embedded in your cornea, do not attempt to remove it. Go directly to the emergency ward at your nearest hospital or see an ophthalmologist. It’s important to seek quick treatment to avoid potentially serious complications, such as an infection, a corneal ulcer or corneal erosion.
Tarsorrhaphy is a surgical procedure that is sometimes performed on patients with corneal exposure or abrasions. The eyelids are partially sewn together to narrow the opening and protect the cornea until healing is complete.
Corneal dystrophy
Treatment may include:
- Lubricating eye drops and ointments: if symptoms are mild
- Glaucoma eye drops: used to reduce the pressure inside the eye (intraocular pressure)
- Temporary eye patch or ‘bandage’ contact lenses: to protect the cornea, increase comfort and facilitate healing
- Excimer laser therapy: can remove abnormalities from the cornea’s surface if symptoms persist
- Corneal transplantation: only in the most severe cases that don’t respond to other treatment
Recurrent corneal erosion
Treatment may include:
- Topical lubricant: This treatment aims to help your epithelial cells heal and regenerate properly
- Antibiotic drops: Depending on the extent of your condition, your ophthalmologist may prescribe antibiotic drops and suggest the short-term use of a therapeutic contact lens, known as a ‘bandage’ contact lens (see below)
- ‘Bandage’ contact lens: These are soft, therapeutic lenses that provide oxygen to the cornea to reduce the risk of corneal hypoxia (insufficient supply of oxygen) and oedema (fluid accumulation). They can also decrease pain and help with the administration of eye drops
- Alcohol delamination: Involves gentle removal of the loose surface epithelium of the cornea to allow new cells to grow and bond with the surface layer
- Phototherapeutic keratectomy (PTK): This surface laser treatment may be recommended if your episodes worsen or become more frequent.
Corneal ulcer
Treatment will depend on the severity and type of corneal ulcer and usually involves antibiotic eyedrops or ointment in the first instance. If the ulceration is in the centre of your eye, it may take longer to recover. An anti-fungal agent may be necessary if the ulcer was caused by a tree branch or dirt.
Corneal transplantation is reserved for severe cases that have failed to respond to other treatments.
Keratitis
Infectious keratitis requires urgent attention.
There are a number of ways to treat keratitis, depending on the cause. Your ophthalmologist will typically prescribe antibacterial, antifungal or antiviral eye drops or ointments to treat the infection.
Prescription eye medication, oral medication or, in some cases, intravenous therapy may be used for more severe cases.
Ocular herpes
While it’s not possible to cure ocular herpes, there are a number of treatments which may help manage or control the condition.
- Ointments: These are used to treat superficial infections. If you wear contact lenses, you will need to stop using them during treatment.
- Debridement: This involves the removal of infected corneal epithelial cells using a cotton swab or corneal spatula.
- Steroid eye drops: These can lessen scarring and infection if the infection is deeper in the corneal layers. Steroid drops must be prescribed by an ophthalmologist because the eye’s natural immune system can be compromised.
- Surgery: This may be recommended for a persistent infection, which can lead to serious scarring if left unresolved.
QLD
SA
VIC
-

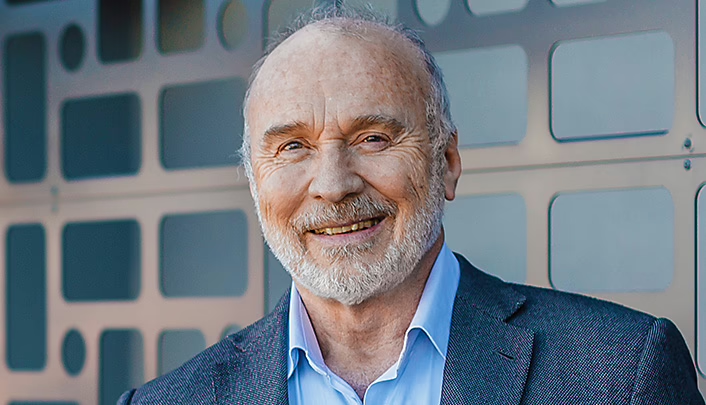
Dr Uday Bhatt
MBBS DTMH DO MSc(EBP) FRCSEd FRCOphth FRANZCO
Locations
- Camberwell
- Coburg
- Footscray
Book a consultationwith Dr Uday BhattResourcesThe information on this page is general in nature. All medical and surgical procedures have potential benefits and risks. Consult your ophthalmologist for specific medical advice.
Date last reviewed: 2025-02-28 | Date for next review: 2027-02-28